Liver Transplantation
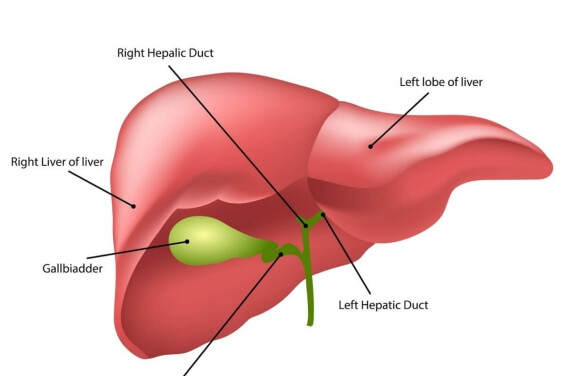
Functions of Liver
Liver performs a myriad of metabolic functions unmatched by any other organ in our body.
The main functions of liver are:
- Produces bile which helps in digestion of fat.
- Synthesis and breakdown of carbohydrates (glycogen)
- Excretion of ammonia as Urea.
- Metabolism and excretion of drugs and toxins.
- Storage of fat soluble vitamins.
Indications
The common indications of liver transplant in children include cholestatic liver disease (most common of which is biliary atresia) and metabolic liver disease followed by acute liver failure. Occasionally it is indicated for liver tumor and certain rare condition.
What are the indications of liver transplatation in children and adolescents?
Indications for liver transplantation are:
- Cholestatic liver disease: Biliary atresia, Alagille’s, syndrome, Progressive familial intrahepatic cholestasis(PFIC), Neonatal hepatitis.
- Metabolic liver disease : Wilson’s disease, Tyrosinaemia, Glycogen storage disorder, Galactosemia, Fatty liver disease, Fatty acid oxidation defects, Bile acid disorders, a1 anti trypsin deficiency.
- Hepatitis : Viral hepatitis (A,E,B,C others), Autoimmune hepatitis, Drugs and poisoning ( including paracetamol poisoning/ toxicity secondary to antituberculosis/antiepileptic drugs).
- Metabolic and Genetic disorders: Metabolic disease where liver is the calpirt. Criggler-Najjar syndrome type-1, Organic acidemias,Urea cycle defects like maple syrup urine disease (MSUD) and Primary oxalosis.
- Liver tumors: Benign tumors that have replaced the whole liver, Unresectable malignant, without extrahepatic metastasis.
Certain rare condition such as factor VII deficiency, Protein C and Protein S deficiency and familial hypercholesterolemia.
Who can Donate Liver
Willing, family donor with matching blood group. The donor should provide an informed consent and also must undergo psychological evaluation. The donor should be 18-55 years old, weighing 55 – 85kg but not fat, should be healthy with normal liver and kidney functions, HBsAg, HCV and HIV negative. It is very important that the donor liver is not fatty therefore a plain CT scan is performed first to calculate the LAI (liver attenuation index). This should normally be more than 6. One would accept a liver with a positive LAI (as compared to spleen). Occasionally a liver biopsy may be done to rule out fatty liver. The donor undergoes complete evaluation of heart, lungs, kidney and other organs., besides a psychiatric evaluation. A CT scan is carried out on the donor to evaluate vascular anatomy and graft volume. MRI (MRCP) provides information of the biliary ducts.
Why is CT scan Triphasic Angiography carried out on the donor?
A CT scan triphasic angiography provides information on the vascular anatomy which is important for the surgeon to know and volumetry is performed on donor liver by using special software which calculates the volume of various parts of the liver.
Who much liver is to left behind with the donor?
At least 35% of the liver is left behind with the donor. For this volume calculation CT volumetry is very important.

What does Pre Transplant Evaluation include?
Immunizations Pre transplantation:
Most units including ours consider live vaccines to be contraindicated after liver transplant because of the risk of dissemination secondary to immunosuppression. It is therefore better to complete normal immunizations before transplant. These include – BCG, DPT + Hib, Hepatitis B, Measles, MMR. Its suggested to give even optional vaccine such as Hepatitis A, Typhoid, chickenpox, influenza rotavirus and pneumococcal vaccines.The vaccination schedule may be expedited and may differ from the normal recommendations
Management of hepatic complications:
It is important to ensure that specific hepatic complications are appropriately managed while the patient waits for transplant. These include portal hypertension, oesophageal varices, ascities, hypoproteinemia etc.
Nutritional support:
It has been demonstrated in several studies that nutritional status at liver transplant is an important prognostic factor in survival, that is better outcome is seen in patients with good nutritional status. The patient needs to be on a high calorie diet (150- 200% calories with good protein intake) with two times the RDA of multi vitamins and in patients with cholestasis supplementation with fat soluble vitamins like vitamin A,D,E,K is done. In patients with cholestasis,MCT oil as in coconut oil is used for cooking. If a child is not able to feed well orally then tube feed supplementation is done, which could be for overnight feeds or during the day as per the need.
Liver Transplant Surgery
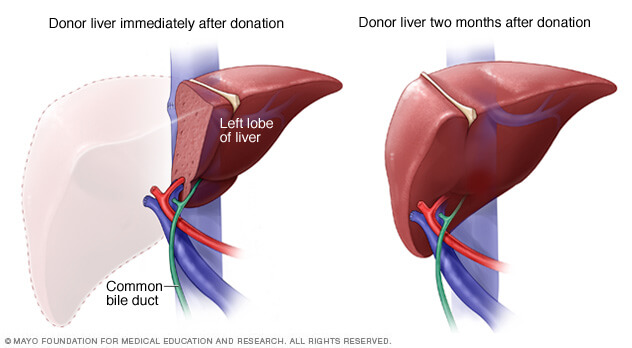
How is Liver Transplant Surgery done?
The surgery takes 8-10 hours.
The donor operation is started first and soon the recipient operation is started. Both surgeries are going on simultaneously in 2 parallel operating theatres. A part of the liver of the donor (usually the left lobe or the left lateral lobe is used in case of a child and right lobe is used in adolescents / adults). The deceased / bad liver of the patient is removed and the part of donor liver is placed in its place. Three important ligations include that of artery vein and duct and in those with previous Kasai’s portoenterostomy, and small children roux-en-Y-jejunostomy is carried out instead of duct to duct anastomosis.
Life after Transplant
Immunosuppression:
Following liver transplant the patient requires immunosuppression usually for life long (according to the present consensus). There are 3 drugs, tacrolimus, mycophenolate mofetil and steroids. Steroids are discontinued first followed by mycophenolate mofetil. Thereafter patient is on 1 immunosuppressive drug, usually tacrolimus, which needs to be taken twice a day daily. The patient needs to undergo regular blood tests to monitor the liver functions, kidney functions and immunosuppressive drug levels.
What’s Life after Liver Transplantation?
Children who survive liver transplant will usually achieve a normal lifestyle despite the necessity for continuous monitoring of immunosuppressive drug levels. They attend normal school sports, activities etc.




Our Experience
We have completed >200 Pediatric Liver Transplants in small children and are the busiest center in India with success rate of 92% at 1 year and overall success rate of over 90% on a median follow up of >4 years.
Our Experience indications of pediatric liver transplantation-
- Cholestatic liver disease is the commonest cause of Liver Transplantation. This includes Biliary atresia, Carolis disease, Allagille Syndrome, Progressive familial intrahehepatic cholestasis (PFIC)Sclerosing cholangitis including Langerhans cell histiocytosis (LCH). Langerhans cell histiocytosis (LCH) is a rare condition of Liver disease secondary to Sclerosing cholangitis and we have 5 year survival of 100% in these patients
- Metabolic Liver Disease – Wilson Diseases is the commonest cause in Metabolic Liver disease that have been transplanted. We have a large experience of other metabolic conditions such as Tyrosinemia, Gyclogen storage disorder (GSD), Maple Syrup Urine Diseases (MSUD), Progressive familial intrahehepatic cholestasis (PFIC), factor VII deficiency & protein C and S deficiency.
- Our team has a good experience of Combined Liver Kidney transplantation in Primary Hyperoxaluria in children with 100%results.
- We have experience in Liver Transplantation in Metabolic inborn errors of metabolism such as MSUD, Citrullinemia etc.
- Acute Liver failure (ALF) and Acute on Chronic liver failure (ACLF) constitutes one third of our total transplants. We have advanced Management Statergy to care in ALF & ACLF patient like Intracranial Bolt in ALF, hemo-dialysis, CRRT, plasma- pheresis, MARS etc. Common causes of ALF are Viral Hepatitis A/E, drugs (ATT) and ACLF are, Wilson disease, tyrosinemia and autoimmune liver disease.
- We have also large series of liver transplant with autoimmune liver disease including autoimmune sclerosing cholangitis.
- We have done surgical innovations to answer shortage of organs such as
- ABO incompatible Liver transplantation – where blood group of donor and recipient is not matching.
- Swap liver transplants– It is a method to match the blood group incompatible donor and recipient couples with another donor and recipient having similar issues.
- Domino liver transplants– In a domino Liver transplant, the explanted liver from a patient who has an illness curable by liver transplant, is used as domino graft for some other patient, as the explanted liver is otherwise well.
- Hepatopulmonary syndromeis a rare complication of Portal hypertension where there is lung failure in association with liver disease. We have transplanted 8 such cases with excellent results.
About
Dr. Neelam Mohan is one of the few women doctors in India who has balanced the various pillars of medical profession and is appreciated as an astute clinician/ healer, bright teacher, researcher, efficient leader/ administrator and for her contribution in social work. She has to her credit many achievements that has put the country on the global medical map.
Services
Copyright 2019 Drneelammohan.com. All rights reserved.

