Pediatric Gastroenterology
Dr. Neelam Mohan
A Pioneering Leader in Pediatric Gastroenterology, Hepatology, and Nutrition,
with over 25 Years of Expertise in the Field
Best Pediatric Gastroenterologist in Delhi NCR
Dr. Neelam Mohan is the Best Pediatric Gastroenterologist in Delhi NCR with an experience of 25 year in her field. She is a pioneer in her field of expertise as a Pediatric Gastroenterologist and liver specialist. She has received the BC Roy National Award from President of India for her pioneering work and novel contribution in the above field to improve the health of children. A Best Pediatric Gastroenterologist in Delhi NCR is a doctor who diagnoses issues related to food pipe, stomach, liver, pancreas and liver, gall bladder and bile duct.
Various problems dealt are:
Gastro-esophagus reflux diseaseVomiting, Nausea, Diarrhea, Constipation, Pain abdomen (Acute / Chronic), Poor appetite, Not growing well in weight or height, Obesity, Malnutrition, failure to thrive, Jaundice, Gall stone, CBC Stone, Biliary atresia, Pancreatic insufficiency, Celiac disease, Food allergy, Appendicitis, Lymph- nodes in abdomen, Tumors in abdomen, Liver tumors, Irritable bowel syndrome (IBS), Inflammatory bowel disease (IBD), Hemorrhoids, Colonic polyps, Anal fissure, Corrosive poisoning, Foreign body ingestion

She has trained several doctors and received the distinguish Teacher Awards by National Board of Examination. In addition a pediatric gastroenterogists performs endoscopy /ERCP. Dr. Neelam Mohan was first in India to start therapeutic endoscopy in newborn and small children and has a vast experience in it.
So, if you’re wondering which Gastroenterologist to see for your children, Dr. Neelam Mohan is unquestionably the Best Pediatric Gastroenterologist in Delhi NCR.
Types of
Gastrointestinal Diseases
Abdominal Pain
Abdominal pain is discomfort or pain felt in the area between the chest and pelvis, often caused by digestive issues or other issues
Diarrhea
Diarrhea is the condition characterized by frequent, loose, and watery bowel movements
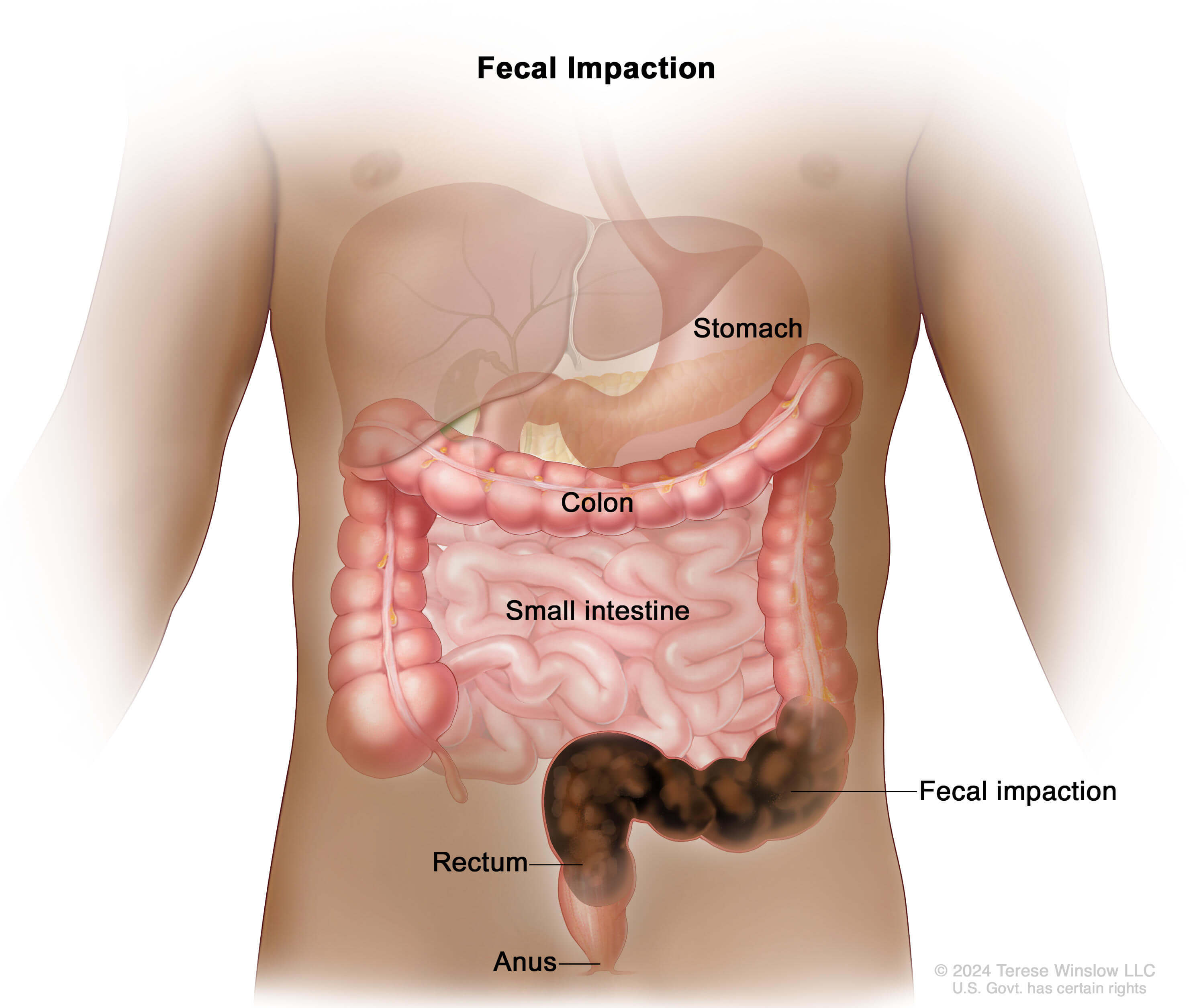
Constipation
Constipation is a condition where a person experiences infrequent, difficult, or painful bowel movements, often accompanied by hard stools
Vomiting
Vomiting is the forcible expulsion of stomach contents through the mouth, often due to illness or irritation
Abdominal Distension
Is the noticeable swelling or enlargement of the abdomen, often caused by gas, bloating, or digestive issues
Difficulty in Swallowing / Dysphagia
Is a condition where a person experiences discomfort or pain while trying to swallow food, liquids, or saliva.
GI Bleed
Is the loss of blood from the digestive tract, which can manifest as vomit or stool that is bloody or dark in color
Celiac Disease
Is an autoimmune disorder where the ingestion of gluten damages the small intestine lining, impairing nutrient absorption
Pancreatitis
Pancreatitis is the inflammation of the pancreas, often causing abdominal pain, nausea, and digestive issues
Inflammatory bowel disease
Inflammatory bowel disease (IBD) is a group of chronic disorders, including Crohn's disease and ulcerative colitis, that cause inflammation in the digestive tract

Experts may very occasionally ask for CT scan and MRI. These are not very routine tests in children.
One needs to approach a specialist like a pediatric Gastroenterologist for pain abdomen in children who would be able accurately assess and manage. Dr. Neelam Mohan has a very vast experience in tackling pain abdomen in children and her results are phenomenal in this field.
Did you know?
Pain abdomen can also result from –
Constipation
Milk intolerance
Psychological stress
Abdominal Migraine / Epilepsy
Food intolerance.
Children can also suffer from ulcer disease.
Abdominal Pain
There are several causes of pain abdomen in children – they could result from causes within the abdomen which could be within or outside the gastrointestinal tract or radiating pain from spine/chest.
Depending on the site of the pain the doctor decides to investigate. The common causes for pain abdomen in children include infections, worms ,gastritis, ulcer disease, reflux disease, constipation, celiac disease, milk intolerance , gall bladder stones/renal stones and inflammatory bowel disease (IBD). Also urine infection may give to lower abdomen it.
Appendicitis, pancreatitis, cholecystitis perforation of gut, lead to acute and severe pain.
Pain abdomen could also be due to conditions like irritable bowel syndrome, abdominal migraine / epilepsy and psychological reasons. They may not be any obvious worrying cause of pain abdomen when its referred to functional abdominal pain.
Rarely it could result from tumors in abdomen. Any causes related to livers kidney pancreas can give rise to pain abdomen, Gynaecological causes usually lead to lower abdominal pain.
The investigations that can be asked for – are blood tests, urine/stool tests, x-ray abdomen and ultrasound abdomen. An endoscopy may be asked for rule out gastritis/ ulcer disease or malabsorption secondary to celiac disease/giardiasis.
Diarrhea
Types of diarrhea:
Diarrhea: Diarrhea is the passage of 3 or more loose or liquid stools per day, or more frequently than is normal for the individual
Persistent Diarrhea: Acute diarrhea episode that lasts for > 14 days.
Chronic diarrhea: diarrhea that lasts for more than 3 weeks.
What is not diarrhea?
Passage of frequent formed stools
Frequent loose greenish yellow stools on D3/D4 of life (Transitional diarrhea)
Passage of pasty stools in a breast fed infant
Passage of stools during / immediately after feeding due to gastrocolic reflex
Diarrhea Continues To Be An Important Contributor to Childhood Deaths in India
NFHS 3: 9% of < 5 suffered from diarrhea in the previous 2 weeks 1
More recent data from UNICEF 10-district survey report that 19.8% children (2-59 months) suffered from diarrhea in the previous 2 weeks
Global & National Diarrhea Treatment Policy
Prevent and treat dehydration with Low osmolarity ORS (or IVF in severe dehydration)
Continue feeding or increase breastfeeding & increase fluids and feeding during and after the diarrheal episode
Give zinc in recommended doses as soon as diarrhea starts
Abstain from giving anti-diarrheal or other drugs
Use antibiotics only when appropriate (i.e. dysentery , systemic infection, cholera, malnutrition)
“Burden” of Diarrhea In India
Burden – 11 % of deaths in the age group of 0–5 years are due to diarrhea
Lancet child survival series, using a prediction model, estimated that estimated 22% (14-30%) of all under-five deaths are attributable to diarrhea in 42 countries, where 90% of all under-five deaths occur
Five countries—India, Nigeria, Democratic Republic of the Congo, Pakistan, and China—contributed to almost half the world’s deaths in children younger than 5 years.
It is estimated that more than 240000 children under 5 years of age die due to diarrhea in India
What Are Our Challenges In The Treatment Of Diarrhea?
Low ORS use rates
Inappropriate management of dehydration
Inadequate emphasis on feeding
Inadequate use of zinc
Irrational use of antimicrobials & other drugs
Hand washing
What is WHO – ORS
WHO ORS : Potentially: “The most important medical advance of this century” – The Lancet
The most important etiology
There is no large-scale comprehensive community based study regarding etiology of diarrhea from India.
Rotavirus is responsible for about 15-30% of episodes in hospitalized children; 7-15% in community.
Almost all episodes leading to hospitalization are reported in children < 2 years.
It is also the most commonly isolated agent in neonatal infections.
Diarrheagenic E. coli is the most common bacterial pathogen.
Shigella sp. is responsible for about 10-20% of episodes. Visible blood is present in stools in half to two-thirds of these episodes.
Vibrio cholerae predominantly occurs in outbreaks. Most affected children are 2-5 yr olds.
Antimicrobials Should be given During Diarrhea Only For: Dysentery, Cholera, Severe Malnutrition, Associated systemic Infection.
Do you know that hand washing is important way to reducing incidence of diarrhea.
Pathogens causing diarrheal diseases.
Mostly transmitted through the feco-oral route Interventions promoting hand washing and other hygiene measures clearly show a reduction in diarrheal risk in the short term
The sustainability of hand washing-behavior in the communities require investigation
The evidence of reduction in risk of diarrheal illnesses after scaling up the intervention in uncontrolled situations is not available
India-specific data on hand washing are scarce
Zinc and Diarrhoea
There is evidence that Zinc supplement in diarrhea can reduce the frequency and severity of diarrhea. Therefore 20mg/day of elemental zinc is recommended in patients with diarrhea for a period of 2 weeks at least. There is some evidence that is can improve the subsequent incidence of diarrhea and pneumonia.
Dysentery
Dysentery is passage of blood in stool resulting from infection . It is usually associated with mucosal stools, abdominal cramps and fever. It is common cause of dysentery are shigella salmonella, E.coli and campylobacter.
Antibiotics are indicated in dysentery.
Probiotic and Diarrhoea
Probiotics are living microorganisms when ingested in sufficient large amount have a health promoting effect on the host.
The various type of probiotics are :-
1) Bacterial Probiotics [Lactobacilli rhamnoses GG, Bifidobacteria, Non-pathogenic E. Coli (E. Coli Nissle 1917), Enterococci (plasmid transfer ++) ]
2) Yeast Probiotic (Saccharomyces boulardii )
Antibiotic drugs and Diarrhea
Watery stools per day and is otherwise unexplained diarrhoea that occurs in association with the administration of antibiotics.
Develop from a few hours up to 2 months after antibiotic intake.
The incidence of diarrhoea varies between different antibiotics.
Drugs that affect the anaerobic flora are prone to cause anti motility drugs.
Rotavirus and Diarrhea
Rota virus diarrhea leads to:
Profuse dehydrating watery diarrhea
Rotavirus is a democratic virus, affects children both in developed and developing countries alike
Hygiene and sanitation make limited difference
It is associated with significant vomiting, making oral rehydration difficult
Evidence that natural infection results in protection
Two natural infections nearly 100% protection against subsequent moderate/severe disease.
But as per recent Indian data even three infections are not 100% protective
Rota virus vaccine mimic protection conferred by natural infection
20% of all deaths in children < 5 years of age from India are due to diarrhea.
Deaths due to rotavirus annually in India : 122,270 and in World : 527,000
Rotavirus accounted for: 39.2% of all diarrhea-related hospital admissions among childern aged < 5 years in India (range from 35% in Mumbai to 53% in Trichy).
23% of deaths due to rotavirus
There are 2 vaccines are available:
Rotaxir (Monovalent) – 2doses
1st dose: age of 6 weeks and no later than at the age of 12 weeks.
The interval between the 2 doses should be at least 4 weeks.
otaTeq (pentavalent) – 3 doses
1st dose: between ages 6–12 weeks
Min interval between doses 4 weeks
3rd dose not after 32 weeks. The manufacturer does not recommend re administration of vaccine if a dose is spit out or regurgitated.
Did you know ?
Rotaviral diarrhea is one of the common causes of watery diarrhea, requiring hospital admission.
Antibiotics are not routinely required in all cases of diarrhea.
We do not like to use drugs like loperamide in diarrhea in children.
Diagnosis
A very good history and clinical examination provides a lot of information. Blood tests and radiological tests such as x-ray and barium may be done to rule out above disorders.
Anal manometry is a useful instrument which is available only at very limited centre such as our and it provides us a lot of information such as
1) First sensation
2) Squeeze pressure
3) RAIR
Which helps to plan management of such cases.
Constipation
Children in India is increasing constipation in rapidly. The incidence has doubled in the last decade. Constipation could broadly be classified into broad categories.
Nerves related cause Hurschsprung’s disease: – The relaxation of muscles is not adequate due to abnormality in the ganglion cells. Constipation starts very early in life in this condition. Usually accompanied by abdominal distension. A barium enema is done followed by anal manometry and rectal biopsy to confirm the diagnosis. If diagnosis is confirmed then a surgery is indicated.
Habitual Constipation – here the underlying cause is not surgery. The constipation usually results secondary to bad dietary habits or post infection.
Constipation may be secondary to hypothyroidism, hypo/hypercalcaemia, vitamin D deficiency, coeliac disease, lactose intolerance/drug induced, irritable bowel syndrome.
Very rarely it may be secondary to motility disorders which are more difficult to treat.
Did you know ?
Bad eating habits can result in constipation.
Excess milk intake in a child may give to constipation
Coeliac disease can not only lead to diarrhea but also constipation.
Vitamin D deficiency can result in constipation.
Constipation can result in tractability lack of confidence, self esteem in a small child.
DO NOT NEGLECT constipation if long standing it will take a long time to resolve
Vomiting
Vomiting is a highly coordinated process in which contents of stomach and upper small intestine are forced out through mouth. Vomiting is caused by a myraid of causes both gastrointestinal and non gastrointestinal. Common causes of vomiting in infant and children are:-
Common GI causes are
Gastroenteritis
GERD – Gastro Esophageal Reflux Disease
Over feeding / forced feeding
Gastritis
Intestinal obstruction
Appendicitis
Hepatitis
Pancreatitis, etc.
Common Non GI causes are:
Systemic infections
Medications
Migraine
Ear, Nose, throat infection
Kidney ailments
Persistent and recurrent vomiting not responding to medication from your pediatrician need to be evaluated by a pediatric gastroenterologist.
Cyclical Vomiting
CVS is characterized by episodes or cycles of severe nausea and vomiting that last for hours, or even days, that alternate with intervals with no symptoms. Although originally thought to be a pediatric disease, CVS occurs in all age groups. Medical researchers believe CVS and migraine headaches are related.
Each episode of CVS is similar to previous ones, meaning the episodes tend to start at the same time of day, last the same length of time, and occur with the same symptoms and level of intensity. Although CVS can begin at any age, in children it starts most often between the ages of 3 and 7.
Episodes can be so severe that a person has to stay in bed for days, unable to go to school or work. The exact number of people with CVS is unknown, but medical researchers believe more people may have the disorder than commonly thought. Because other more common diseases and disorders also cause cycles of vomiting, many people with CVS are initially misdiagnosed until other disorders can be ruled out. CVS can be disruptive and frightening not just to people who have it but to family members as well.
Abdominal Distension
Abdominal distension or swelling of abdomen can result from following common causes in children:
Overweight /obesity (fat)
Hypotonia (Hypothyroid, vitamin D deficiency)
Malabsorption (celiac disease , dysentery etc.)
Mass in abdomen (tumors, cysts, etc.)
Fluid in abdomen
Did you know?
Vitamin D deficiency is common in children in India, despite being a tropical country.
Vitamin D deficiency can lead to hypotonia, abdominal distension, pain in legs/back, tiredness, rickets and growth failure in children.
Difficulty in Swallowing / Dysphagia
This could result from lesions in oral cavity, pharynx or food pipe disorders. Common food pipe or oesophageal causes in children are oesophagitis resulting from gastro-esophageal reflux disease / hiatus hernia/eosinophilic oesophagitis / milk protein allergy or inflammatory disorders.
Sometimes ingestion of acid or alkali can give rise to erosions / ulcers and subsequently oesophageal strictures which can result in dysphagia. Congenital oesophageal narrowing /stenosis or webs can result in dysphagia. If a foreign body gets stuck in oesophagus or food pipe, it can result in dysphagia. Rarely motility disorders and achalasia ((failure or relaxation of gastro oesophageal junction ) can result in dysphagia.
Tumors are not common in children.
Did you Know?
Gastro oesophageal reflux disease (GERD) is also common in infants and young children also. In adults its very common and non medical language used by patients for this symptoms is acidity.
GI Bleed
Blood in child’s vomit or stool can be a sign of gastrointestinal (GI) bleeding. GI bleeding can be scary for you and your child. Many times, the cause of the bleeding is not serious. Still, your child should ALWAYS be seen by a doctor if GI bleeding occurs.
The GI Tract
The GI tract is the path that food travels through the body. Food passes from the mouth down the esophagus (the tube from the mouth to the stomach).
Food begins to break down in the stomach and then moves through the duodenum, the first part of the small intestine.Nutrients are absorbed as food travels through the small intestine. Undigested food passes into the large intestine (colon) as waste.
The colon removes water from the waste. Waste continues from the colon to the rectum (where stool is stored). Waste then leaves the body through the anus.
Celiac Disease
What is Celiac disease?
Celiac disease is a digestive disease that damages the small intestine and interferes with absorption of nutrients from food. People who have celiac disease cannot tolerate a protein called gluten, found in wheat, rye, and barley. Gluten is found mainly in foods, but is also found in products we use every day, such as stamp and envelope adhesive, medicines, and vitamins.
When people with celiac disease eat foods or use products containing gluten, their immune system responds by damaging the small intestine. The tiny, fingerlike protrusions lining the small intestine , called villi, are damaged or destroyed. They normally allow nutrients from food to be absorbed into the bloodstream. Without healthy villi, a person becomes malnourished, regardless of the quantity of food eaten.
Because the body’s own immune system causes the damage, celiac disease is considered an autoimmune disorder. However, it is also classified as a disease of malabsorption because nutrients are not absorbed. Celiac disease is also known as celiac sprue, non-tropical sprue, and gluten-sensitive enteropathy.
Is this disease has genetic tendency?
Celiac disease is a genetic disease, meaning it runs in families. The commonest gene implicated are HLA DQ2 AND DQ8. The incidence of sibling of the index patient developing coeliac disease is ~10%. Sometimes the disease is triggered-or becomes 2 active for the first time-after surgery, pregnancy, childbirth, viral infection, or severe emotional stress.
What are the symptoms of a child with celiac disease?
Symptoms of celiac disease may include one or more of the following:
Recurring abdominal bloating and pain
Chronic diarrhea (constipation in atypical celiac disease)
Pale, foul-smelling, or fatty stool
Weight loss / poor weight gain
Failure to thrive in infants
Delayed growth Fatigue / lethargy
Unexplained anemia ( low hemoglobin levels)
Bone or joint pain
Osteoporosis, osteopenia
Behavioral changes
Tingling numbness in the legs (from nerve damage)
Muscle cramps
Seizures
Missed menstrual periods (often because of excessive weight loss)
Infertility,
Recurrent miscarriage
Pale sores inside the mouth, called aphthous ulcers
Tooth discoloration or loss of enamel
Itchy skin rash called dermatitis herpetiformis
In babies, symptoms may develop after weaning onto cereals which contain gluten. Other symptoms in young children include:
Muscle wasting in the arms and legs
Bloated tummy
Irritability
Failure to gain weight or lose weight after previously growing well Symptoms in older children vary as they do in adults.
What are the clinical manifestation?
The clinical presentation of coeliac disease are classified as typical (presenting with features of malabsorption such as diarrhoea, abdominal distension) or atypical (those cases without diarrhoea. Common presentations with atypical CD include refractory anaemia, short stature, constipation, rickets, pain abdomen.
What test need to be done?
There are specific blood tests used to diagnose coeliac disease. They look for antibodies that the body makes in response to eating gluten. Antibodies are protective proteins produced by the immune system in response to substances that the body perceives to be threatening. Autoantibodies are proteins that react against the body’s own molecules or tissues.
To diagnose celiac disease, physicians will usually test blood to measure levels of:
Immunoglobulin A (IgA)
anti-tissue transglutaminase antibody (tTGA)
IgA anti-endomysia antibodies (AEA)
Before being tested, one should continue to eat a regular diet that includes foods with gluten, such as roti, maida, breads and pastas. If a person stops eating foods with gluten before being tested, the results may be negative for celiac disease even if celiac disease is actually present.
If the tests and symptoms suggest celiac disease, the doctor will perform a small bowel biopsy. During the biopsy, the doctor removes a tiny piece of tissue from the small intestine to check for damage to the villi. To obtain the tissue sample, the doctor eases a long, thin tube called an endoscope through the mouth and stomach into the small intestine. Using instruments passed through the endoscope, the doctor then takes the sample. The procedure is done under-sedation in children and is not painful.
What is the treatment?
The only treatment for celiac disease is to follow a gluten-free diet. A gluten-free diet means not eating foods that contain wheat, rye, and barley. The foods and products made from these grains such as atta, maida sooji, bakery products are not allowed.
Checking labels for “gluten free” is important since many corn and rice products are produced in factories that also manufacture wheat products. Hidden sources of gluten include additives such as modified food starch, preservatives, and stabilizers. Wheat and wheat products are often used as thickeners, stabilizers, and texture enhancers in foods.
Foods To Omit: Bread, cereal
heat, maida, sooji, Barely, oats, rye, malt. Usually all bakery products bread biscuits, burgers, pastas, spaghetti, contain gluten unless specified
Foods To Omit : Vegetable
Any creamed or breaded vegetables (unless allowed ingredients are used); and canned baked beans Some french fries- these are coated with flour
Foods To Omit : Fruits
Some commercial fruit pie fillings
Foods To Omit : Milk Yogurt and cheese
Malted milk , Some milk drinks, flavoured or frozen yogurt which may contain malt
Foods To Omit : Meat, poultry, fish, dry beans and peas, eggs and nuts
Any prepared with wheat, rye, oats, barley, gluten stabilizers, fillers including some frankfurters, cold cuts, sandwich spreads, sausages, canned meats Self-basting turkey.
Foods To Omit : Fats, snacks, sweets, condiments and beverages
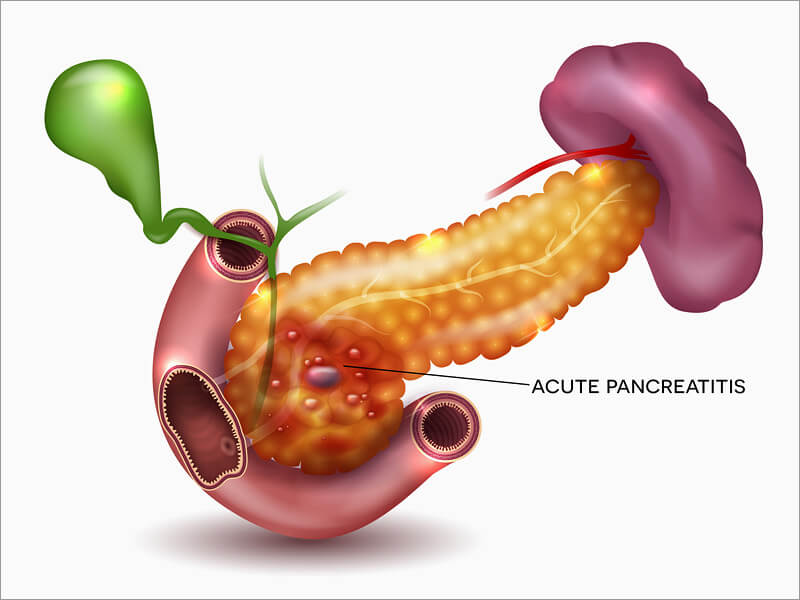
Complications:
The sooner acute pancreatitis is treated, the less likely complications will occur. Complications include:
Damage to the pancreas
Benign growths called cysts can grow in the pancreas
An abscess
A fistula – which is when a channel or hole develops in the pancreas
Bleeding
Blocked blood flow to the pancreas
High blood sugar levels
Cause:
Common causes of acute pancreatitis in children are:
Abdominal injuries
Gallstones in the bile duct – this is the most common cause
Choledochal cyst
Certain medicines (eg. azathioprine, corticosteroids)
Idiopathic
After an ERCP Infection
Increased calcium or lipid (fat) levels in the blood
Pancreas divisum – this is when you are born with ducts in the pancreas which don’t function properly
Genetics – you may inherit a faulty gene from your parents, this is called hereditary pancreatitis
Inflammation of the blood vessels in the pancreas or reduced blood flow to the pancreas
Renal failure
Rarely a tumor
Diagnosis: Besides asking about a person’s medical history and doing a physical exam, a doctor will order a blood test to diagnose acute pancreatitis. A doctor may also order an abdominal ultrasound or a CT scan.
Treatment: Treatment depends on the severity of the attack and hospitalization is required if pain is severe, oral intake is inadequate or any complications are suspected.
Pancreatitis
Since Pancreas is a 15 centimetre (six inches) long organ which is part of digestive system. It’s found just in front of spine (back bone), behind stomach, at the level where the two sides of rib cage join together. It’s connected to the duodenum (small bowel) by a duct (tube) called the pancreatic duct.
Pancreas produces enzymes (digestive juices) which break down food, particularly fatty foods. These digestive juices pass down the pancreatic duct into the duodenum which contains food to be digested. The pancreas also produces insulin, a hormone that helps to keep the level of sugar in blood constant.
If you have acute pancreatitis, the enzymes produced in the pancreas start to digest and damage the pancreas before reaching the duodenum. Pancreatitis is an inflammation of the pancreas.
Acute Pancreatitis:
Acute pancreatitis usually begins with pain in the upper abdomen that may last for a few days. There are a number of symptoms of acute pancreatitis, including:
Severe pain around the upper part of abdomen (tummy) and/or back which is worse when you lie down
Feeling sick
Vomiting
A high temperature
Jaundice – which is when the whites of your eyes and skin look yellowed
Abdomen (tummy) is larger than usual
The skin on lower back or abdomen may be blue-grey
Chronic Pancreatitis:
If injury to the pancreas continues, chronic pancreatitis may develop. Chronic pancreatitis occurs when digestive enzymes attack and destroy the pancreas and nearby tissues, causing scarring and pain. Chronic pancreatitis is rare in children. Trauma to the pancreas and hereditary pancreatitis are two known causes of childhood pancreatitis.
Other causes are congenital conditions such as pancreas divisum , cystic fibrosis, high levels of calcium in the blood, high levels of blood fats, some drugs, certain autoimmune conditions.
Diagnosis: Diagnosis depends on demonstrating abnormality in pancreatic gland or duct. Diagnosis may be difficult, but new techniques can help using ultrasonic imaging, MRCP (MRI) endoscopic retrograde cholangiopancreatography (ERCP), and CAT scans.
Treatment includes relieving pain, a diet low in fat, alcohol must be avoided, +/- pancreatic enzymes supplements. In some cases, ERCP, stenting, lithotripsy or surgery may be required.
Inflammatory bowel disease
Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine. The major types of IBD are Crohn’s disease and ulcerative colitis. Common presentation of these disorders include bleedind per rectum, chronic diarrhea, pain abdomen and growth. Failure. Crohn’s disease and ulcerative colitis may present with extra-intestinal manifestations (such as liver problems, arthritis, skin manifestations and eye problems) in different proportions.
The main forms of IBD are Crohn’s disease and ulcerative colitis (UC) The main difference between Crohn’s disease and UC is the location and nature of the inflammatory changes. Crohn’s can affect any part of the gastrointestinal tract, from mouth to anus (skip lesions), although a majority of the cases start in the terminal ileum. Ulcerative colitis, in contrast, is restricted to the colon and the rectum.
Microscopically, ulcerative colitis is restricted to the mucosa (epithelial lining of the gut), while Crohn’s disease affects the whole bowel wall (“transmural lesions”). Rarely, a definitive diagnosis of neither Crohn’s disease nor ulcerative colitis can be made because of idiosyncrasies in the presentation. In this case, a diagnosis of indeterminate colitis may be made. Although a recognised definition, not all centres refer to this.
Book An Appointment

Get The Right Medical Care
Call Us:
+91 9818200582 / Helpline no. : 01244141414
VISIT US:
Medanta the Medicity:
Sector 38 – Gurgaon; 122001, Monday to Saturday; from 11:00 am to 4:30 pm,
Contact no. 0124-4141414
Medanta Mediclinic, E-18, Golf course road, Gurgaon-110024, Days & Time: Tuesday & Friday, 4:30 pm to 5:30 pm,
Contact no. 011 44114411 / 9818200582
Email: drneelam@yahoo.com
mohanpedgastro@gmail.com

Sr. Director, Dept. Pediatric Gastroenterology, Hepatology, Liver Transplantation,
Medanta - The Medicity, Gurugram
Follow Us
Resource Links
Top Trending Post

council member of FISPGHAN
December 2024

Developed global strategies, guidelines
December 2024
Contact Info

Location
Medanta, the Medicity

Email Us
drneelam@yahoo.com

Phone Us
+91 9818200582
© Copyright 2025 Dr. Neelam Mohan
Designed By netwellify.com